
CHECKLISTS

The Power of Checklists in Healthcare and Beyond
IN ACTION
The Simplest Way To Reduce Complications
Checklists are a powerful tool for any industry concerned with safety measures.
In healthcare, organizations that have implemented checklists have improved risk prevention, reduced errors, and enhanced team collaboration among healthcare providers.
This microsite explores The Surgical Safety Checklist, its history, implementation, and key players like Atul Gawande, Peter Pronovost etc. Inspired by Gawande's book 'The Checklist Manifesto' and other sources, it highlights the impact of checklists in reducing errors and enhancing collaboration among healthcare providers.
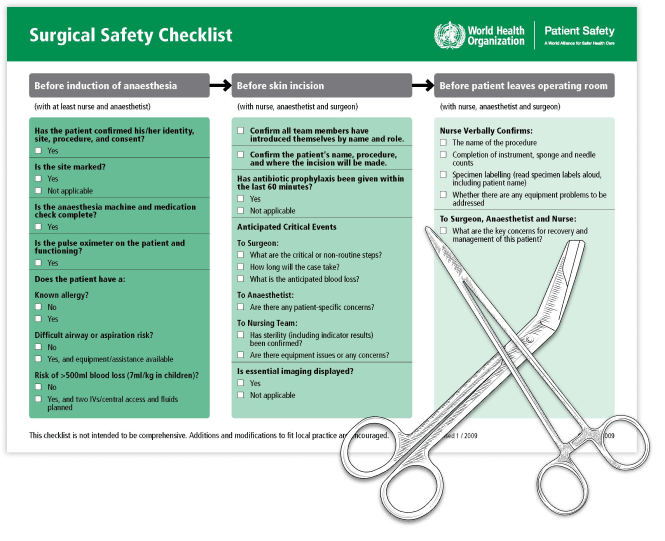
The Surgical Safety Checklist
The WHO developed the Surgical Safety Checklist to decrease errors and adverse events, and improve teamwork in surgery.
The Surgical Safety Checklist is meant to serve as a wireframe, and it is encouraged that hospitals modify and adapt the checklist to their specific environment and culture
The history of checklists in healthcare, leading to the development of the surgical safety checklist, is long and fascinating. This innovative tool is the result of years of effort by healthcare professionals to standardize processes and optimize patient safety.
1960
THE NURSE'S CHECKLIST
Nurses developed patient charts and forms that incorporated the monitoring of four vital signs: body temperature, pulse, blood pressure, and respiratory rate. These tools enabled them to keep track of their patients' health status by regularly checking and evaluating their vital signs every six hours. This system helped ensure that patients received timely and appropriate medical attention when necessary.
2001
PETER PRONOVOST'S CHECKLIST
In 2001, critical care specialist Peter Pronovost introduced a checklist system at Johns Hopkins Hospital's ICU. The system included five simple steps that nurses could use to observe doctors and stop them if they skipped a step. This collaborative approach allowed for effective communication between medical professionals and resulted in a remarkable outcome. Within a year, the rate of ten-day line infections dropped from 11 to 0, preventing 43 infections and eight deaths and saving the hospital $2 million in costs. This success story showcases the importance of implementing checklists and promoting collaboration between medical professionals to improve patient safety.

2003 - 2006
THE MICHIGAN KEYSTONE PROJECT
The Keystone Initiative in Michigan utilized a checklist system to enhance patient safety in ICUs. Each participating hospital appointed a project manager and a senior executive to troubleshoot any issues through conference calls with Peter Pronovost. Within three months, the infection rate in Michigan's ICUs dropped by 66%, saving more than 1500 lives and reducing costs by roughly $175 million. These remarkable results were published in the New England Journal of Medicine in 2006, emphasizing the significance of collaboration and evidence-based tools, such as checklists, in healthcare to improve patient safety.
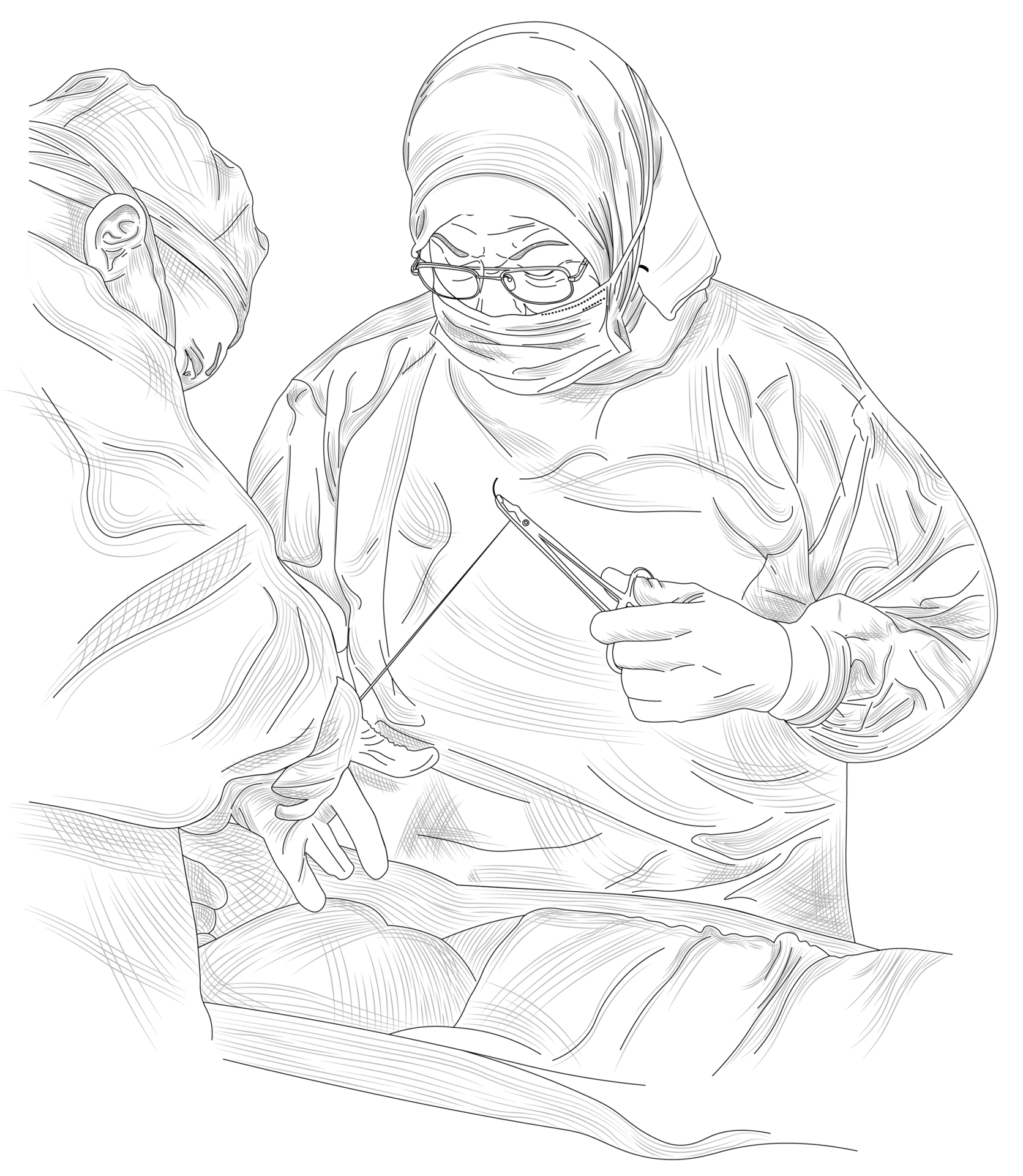
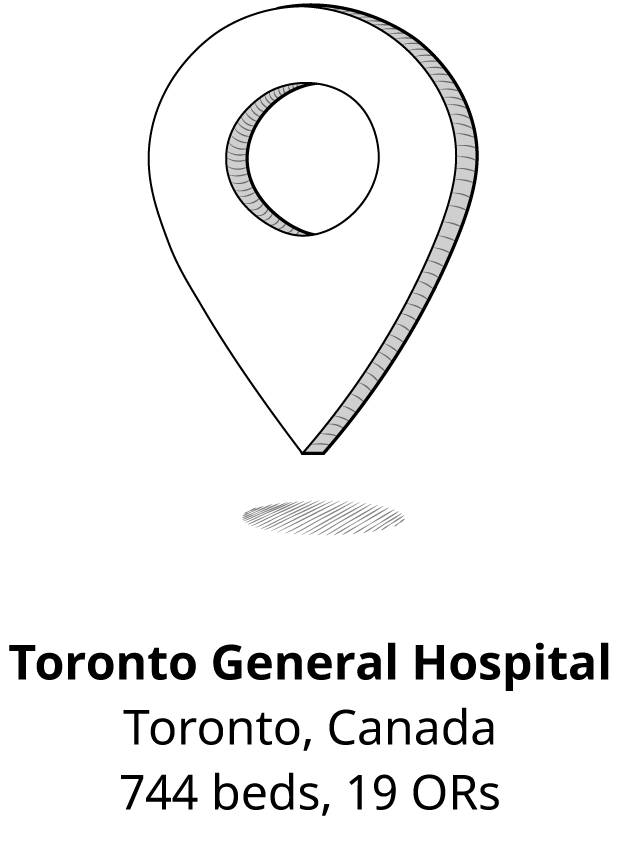
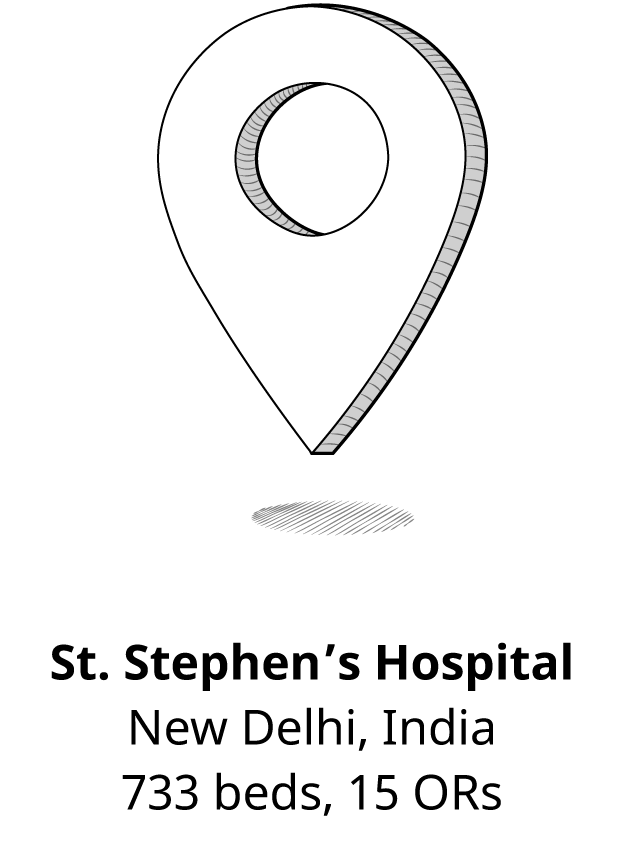
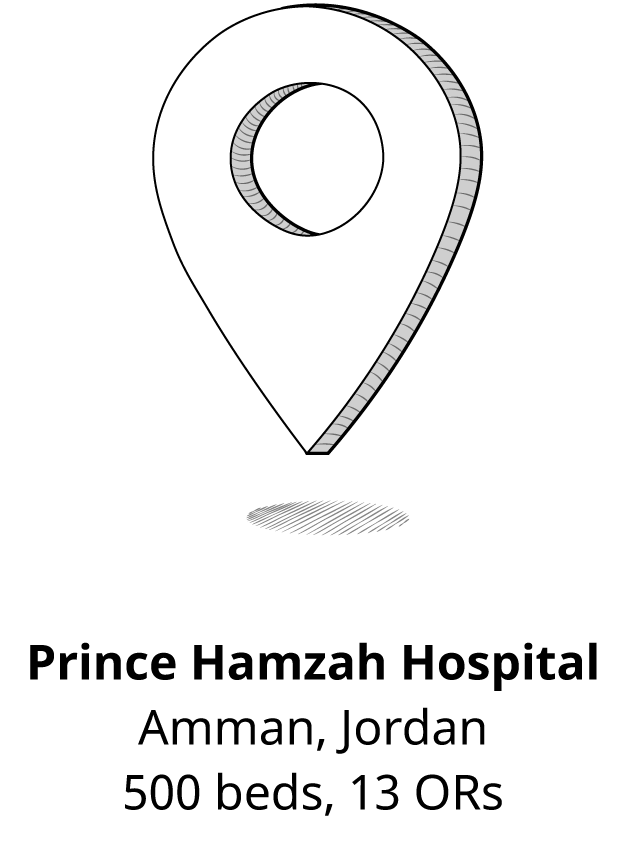
SAFE SURGERY SAVES LIVES
To enhance patient safety and implement safer surgical procedures, a global research team launched a project aimed at reducing adverse events in both operating rooms and wards. The team selected eight hospitals across the world. This initiative reflects the importance of a global approach to patient safety, utilizing evidence-based practices and collaboration to improve outcomes in healthcare settings worldwide.
2007 - 2008

2009
WHO'S OFFICIAL
SURGICAL SAFETY CHECKLIST
After extensive research spanning several years, the World Health Organization developed a surgical safety checklist in 2009 that healthcare workers worldwide use in their operating rooms today. This standardized and universal checklist has become an essential tool for ensuring patient safety during surgical procedures, reflecting the WHO's commitment to improving healthcare outcomes globally.
The Essential Role of Checklists Across Industries


The history of checklists in healthcare, leading to the development of the surgical safety checklist, is long and fascinating. This innovative tool is the result of years of effort by healthcare professionals to standardize processes and optimize patient safety.
1960
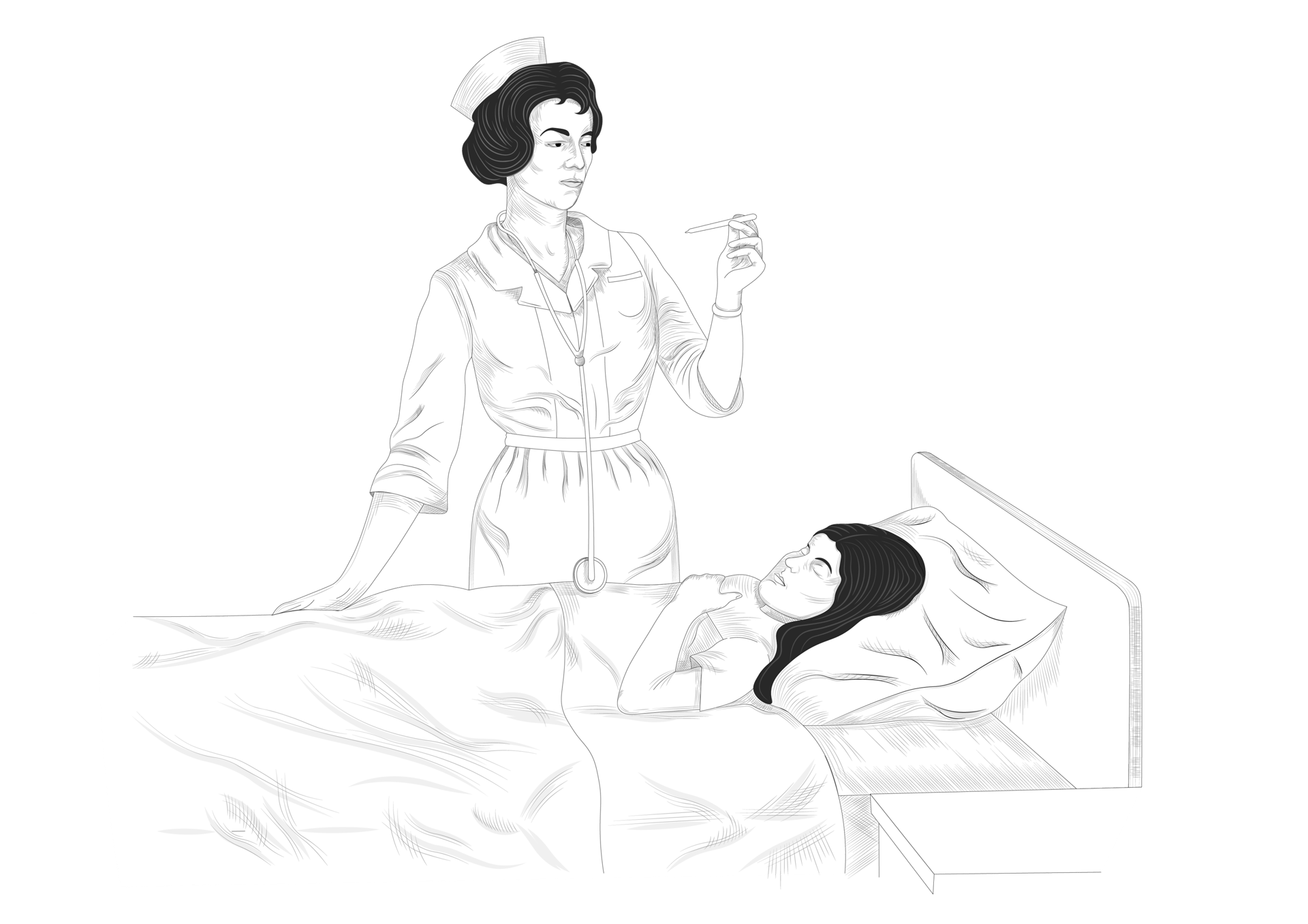
Nurses developed patient charts and forms that incorporated the monitoring of four vital signs: body temperature, pulse, blood pressure, and respiratory rate. These tools enabled them to keep track of their patients' health status by regularly checking and evaluating their vital signs every six hours. This system helped ensure that patients received timely and appropriate medical attention when necessary.
THE NURSES’ CHECKLIST
2001
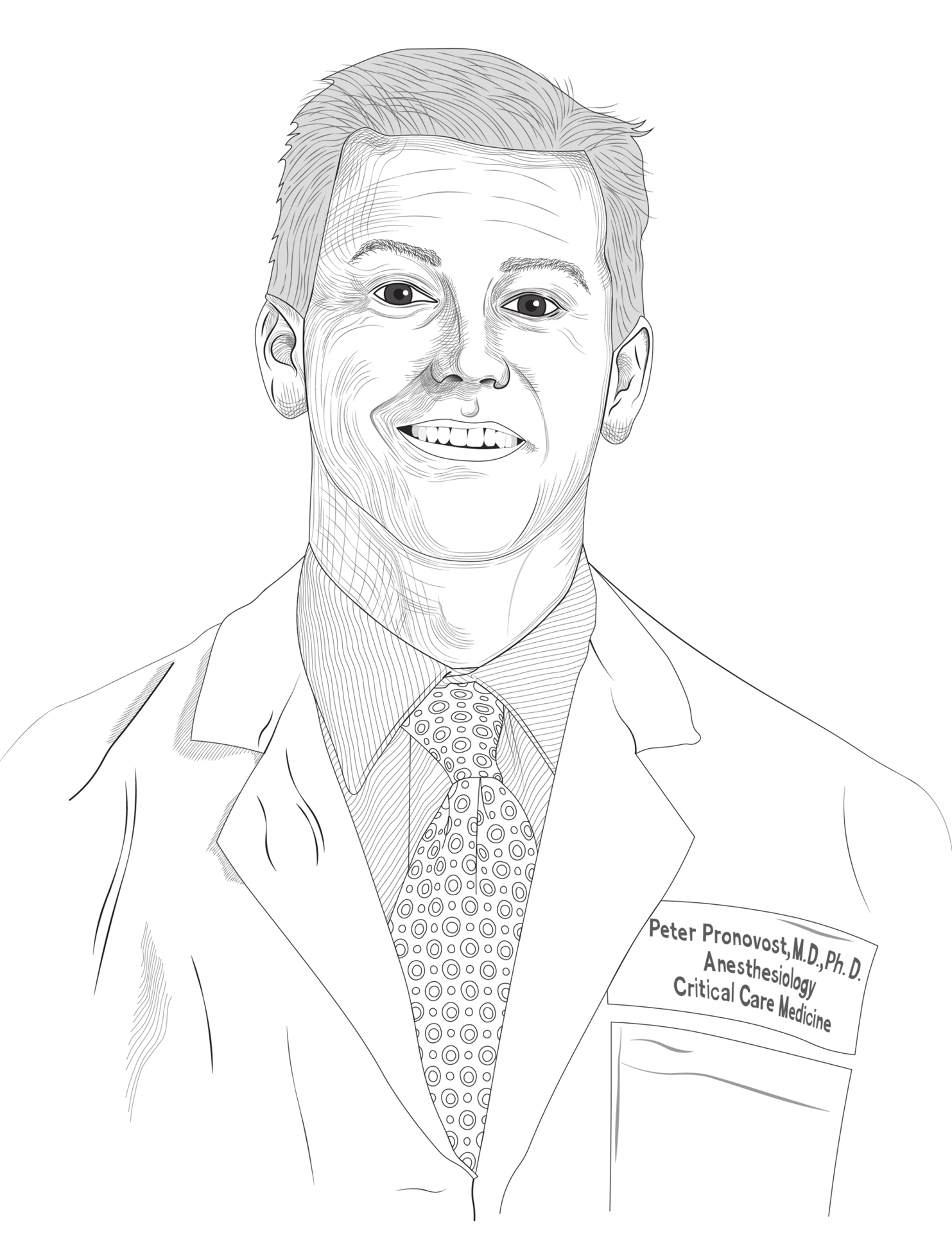

In 2001, critical care specialist Peter Pronovost introduced a checklist system at Johns Hopkins Hospital's ICU. The system included five simple steps that nurses could use to observe doctors and stop them if they skipped a step. This collaborative approach allowed for effective communication between medical professionals and resulted in a remarkable outcome. Within a year, the rate of ten-day line infections dropped from 11 to 0, preventing 43 infections and eight deaths and saving the hospital $2 million in costs. This success story showcases the importance of implementing checklists and promoting collaboration between medical professionals to improve patient safety.
PETER PRONOVOST'S CHECKLIST
2003 - 2006
The Keystone Initiative in Michigan utilized a checklist system to enhance patient safety in ICUs. Each participating hospital appointed a project manager and a senior executive to troubleshoot any issues through conference calls with Peter Pronovost. Within three months, the infection rate in Michigan's ICUs dropped by 66%, saving more than 1500 lives and reducing costs by roughly $175 million. These remarkable results were published in the New England Journal of Medicine in 2006, emphasizing the significance of collaboration and evidence-based tools, such as checklists, in healthcare to improve patient safety.
THE MICHIGAN KEYSTONE PROJECT
2007 - 2008
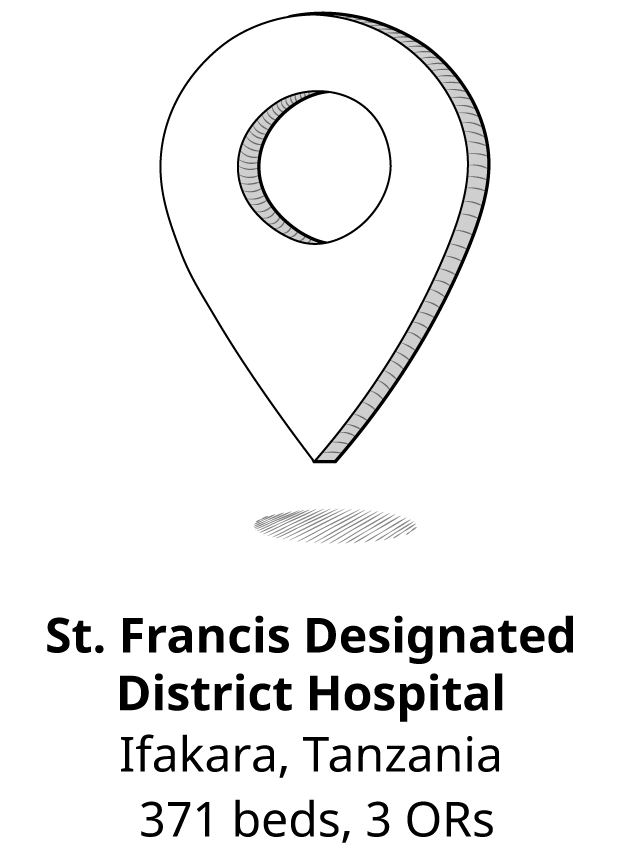
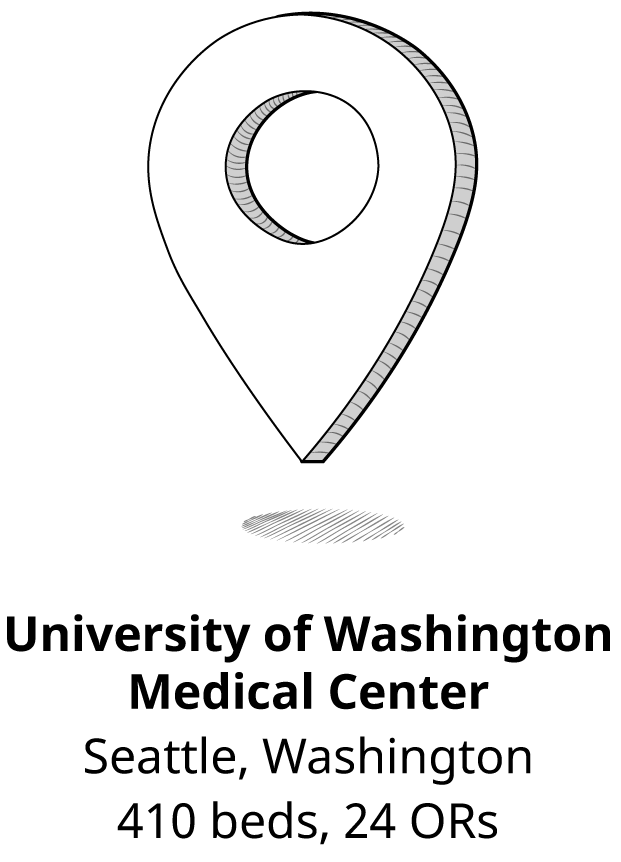
To enhance patient safety and implement safer surgical procedures, a global research team launched a project aimed at reducing adverse events in both operating rooms and wards. The team selected eight hospitals across the world. This initiative reflects the importance of a global approach to patient safety, utilizing evidence-based practices and collaboration to improve outcomes in healthcare settings worldwide.
SAFE SURGERY SAVES LIVES
After extensive research spanning several years, the World Health Organization developed a surgical safety checklist in 2009 that healthcare workers worldwide use in their operating rooms today. This standardized and universal checklist has become an essential tool for ensuring patient safety during surgical procedures, reflecting the WHO's commitment to improving healthcare outcomes globally.
WHO'S OFFICIAL SURGICAL SAFETY CHECKLIST

2001
The Surgical Safety Checklist is not a cure-all solution but a tool for safer surgery. Ultimately, it is up to each organization and hospital to ensure they are abiding to the checklist as close as possible.
Teamwork & Discipline
Aviation
Industries
The Essential Role of Checklists in Other Industries
Construction
Nuclear Power
Healthcare
Space Exploration
OBSTACLES
Factors That Affect Successful Utilization of the Checklist
By providing practitioners with the ability to evaluate their team's performance, the checklist facilitates team communication within a non-punitive environment.
The OR Black Box® Impact
CULTURE
In the operating room , healthcare providers often encounter hierarchy as a significant obstacle to successful checklist implementation. Fear of speaking up, intimidation, and ingrained cultural biases can undermind the effectiveness of the Checklist.
By utilizing the checklist as a dynamic and customizable tool, hospitals can adapt and establish their own milestones. Successful compliance varies based on the unique resources and size of each hospital, allowing for tailored implementation.
The OR Black Box® Impact
COMPLIANCE
Monitoring compliance and fostering staff commitment are essential for the effectiveness of the checklist. Healthcare providers should feel supported throughout the process, and any workflow disruptions or work overload should be promptly addressed. It is important to remember that the checklist serves as a tool for promoting safety and communication, rather than functioning as an instruction manual.
Clark, Andrew (January 15, 2009). "Plane crashes in Hudson river in New York". The Guardian – via www.theguardian.com
Gawande, Atul (2009). The Checklist Manifesto.
Hecla, Jake et al. (August 31, 2020). “Minimizing the consequences of nuclear accidents through effective communication”. Bulletin of the Atomic Scientists.
Lifebox and Ariadne Labs (2019). “Checking In On the Checklist: Uptake, Impact, and Opportunities for the Next Decade”.
Marshall, Richard D.; et al. (May 31, 1982). "Investigation of the Kansas City Hyatt Regency Walkways Collapse". NIST. Building Science Series. U.S. Dept. of Commerce, National Bureau of Standards.
Matthew Hersch (July 19, 2009). “The Fourth Crewmember”. Smithsonian Magazine.
Montgomery, Rick (July 15, 2001). "20 years later: Many are continuing to learn from skywalk collapse". The Kansas City Star.
WHO. Safe Surgery. Surgical Safety Checklist.
